Blog

New Pricing on Abena!
We are happy to announce new sales on Abena Abri-Flex Level 3 and Abena Abri-Form Level 4. Take advantage of our new prices and SAVE.

Proper Way To Put On Disposable Adult Diapers and Pull-Up Underwear - Abena Diapers
We receive questions daily regarding how to properly put on disposable adult diapers and pull-up underwear. These four video's from Abena do an excellent job demonstrating the proper way to put...

Abena Product Review
The Abena brand offers some of the most absorbent disposable protective diapers/briefs and pull-up underwear on the market today. Abena is known as one of...
3 Basis Types of Bladder Control Issues
The 3 Basis Types of Bladder Control Issues: 1) Stress You leak unexpectedly when you laugh, cough, sneeze or do physical activity. Weakened bladder muscles...
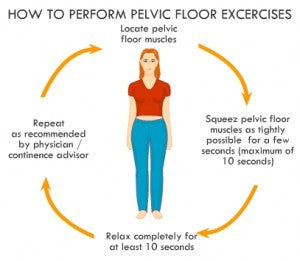
Exercises for Urinary Stress and Urge Incontinence
The exercises most effective for Urinary Stress and Urge Incontinence are known as pelvic floor exercises or Kegel exercises. These exercises help to strengthen the...

Method to Save on the Cost of Incontinence Supplies Through HSA, FSA or HRA.
Now that 2011 is coming to an end many Americans are beginning to think about filing taxes and looking to ensure they utilize their health...

eMedical, Inc. – Newly Designed Site at emedicalnow.com
Thank you for taking the time to visit our newly designed site at www.emedicalnow.com and my blog. We have redesigned our site to improve the...
